Blepharokeratoconjunctivis
Note: This condition requires an in person, comprehensive eye examination with a licensed eye care practitioner (optometrist or ophthalmologist) for diagnosis.
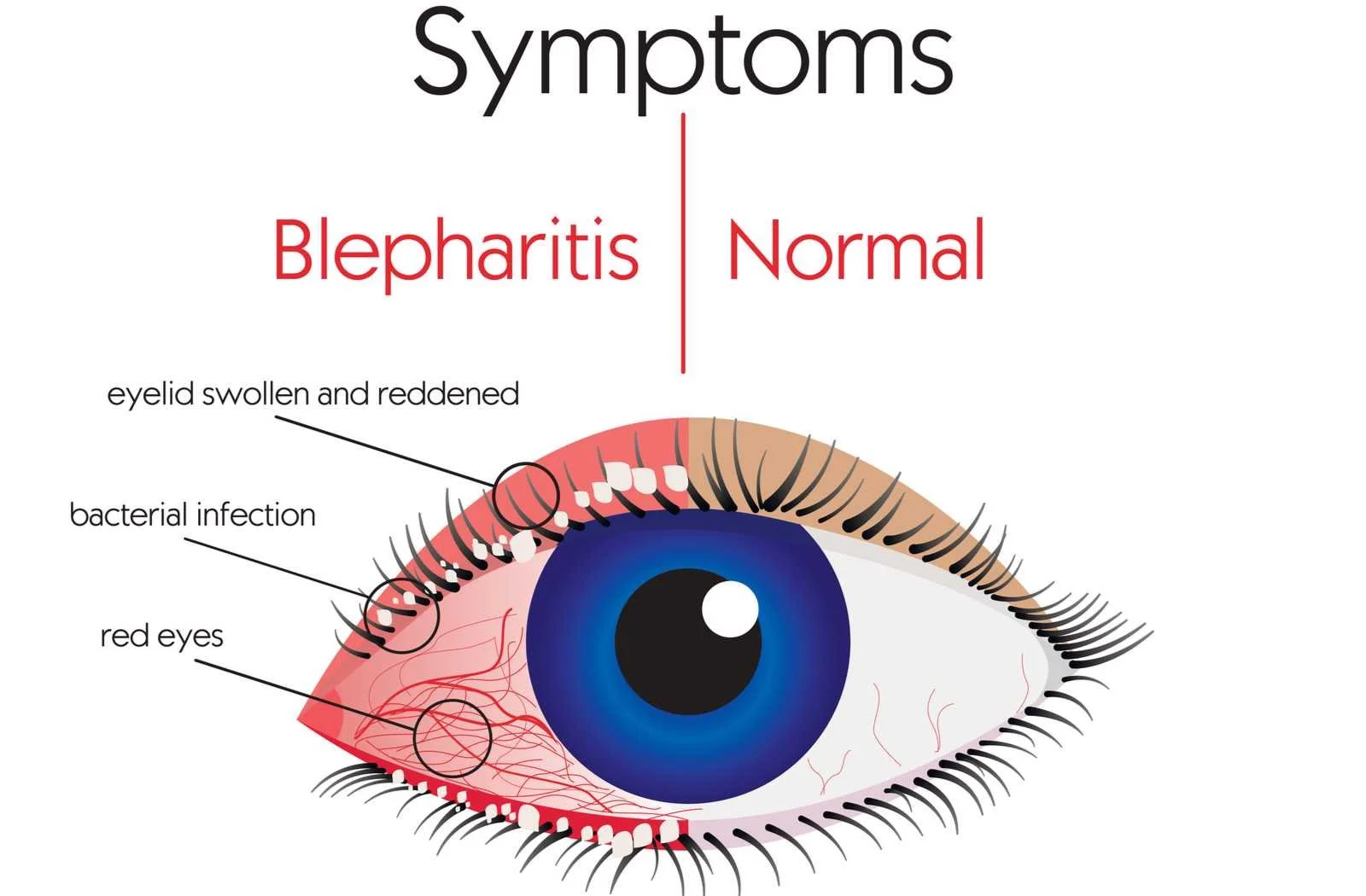
Blepharokeratoconjunctivitis (BKC) (also known as Marginal Keratitis) is a chronic inflammatory disorder primarily affecting the eyelids with secondary involvement of the conjunctiva and the cornea.
The conjunctiva and the sclera make up the white part of the eye
The cornea is the clear window on the front of your eye
When only the eyelids are involved, the condition is called “Blepharitis”, meaning inflammation of the eyelids. When the cornea and conjunctiva are affected, the condition is called “Blepharokeratoconjunctivitis” or “Marginal Keratitis”. BKC is a more serious condition because corneal scarring and abnormal blood vessel growth can lead to decreased vision/visual impairment.
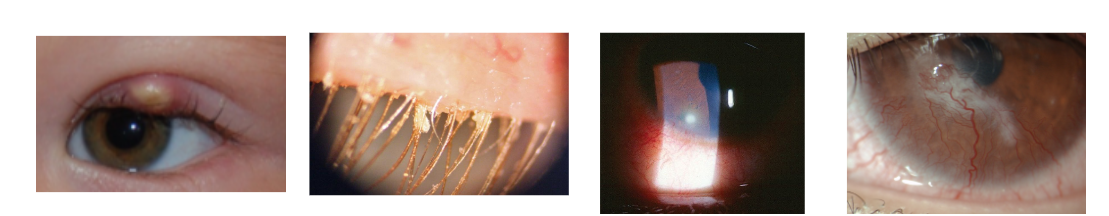
Your eyelids contain tiny glands that make oil which keeps your eyes moist. In blepharitis, these glands become blocked, which causes your eyelids to become irritated and some children get styes/bumps in their eyelids. In some cases, dandruff-like flakes build up at the base of the eyelashes. It is thought that in some children blepharitis is caused by sensitivity to the bacteria (staphylococcus) which normally live on the skin. The surface of the eye can become inflamed. The eye becomes red and sore and may develop small white ulcers around the edge of the cornea.
Signs of BKC
Eyelash crusting
History of styes/chalazia
Redness
A white or yellow nodule on the cornea or conjunctiva
Symptoms of BKC
Irritation or itchiness
Foreign body sensation
Tearing
Light sensitivity
Decrease in vision
Treatment
In order to decrease the ocular surface inflammation, you should develop a consistent, daily lid hygiene routine to treat the blepharitis. This is especially important for preventing BKC from recurring. A good lid hygiene regimen includes: 1) Warm compresses 2) Lid massage 3) Lid scrubs. Additionally, your eye doctor may recommend eye drops (may be prescription or non prescription).
Warm compresses
Purpose: This melts the oily secretion blocking the openings of the glands and softens any lash flakes.
Instructions:
Heat a clean gel or bead mask in the microwave. Alternatively use a sock and fill it with uncooked rice and heat it in the oven or microwave.
Hot wet towels are also an option, however, you should prepare several as they tend to lose heat quickly.
Apply the compress gently over closed eyelids for 15 minutes per session, reheat when warm.
Perform 4 times per day if there is an eyelid bump, then 1-2 times per day for maintenance.
Commercially available warm compress brands: Thermalon, Bruder Mask, TranquilEyes
Youtube Video by UC Berkeley “Meibomian Gland Dysfunction Home Therapy” UC Berkeley” https://www.youtube.com/watch?v=F4SjQrNByok&t=7s
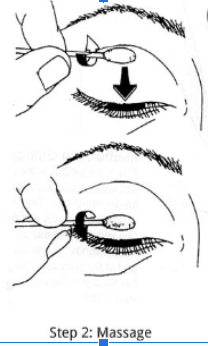
Lid Massage
Purpose: This helps to push out the oil from the tiny eyelid glands.
Instructions:
Wash your hands thoroughly
Remove the warm compress and gently massage the lower lid near the lid margin with your finger, rolling your finger upward in a rolling motion (do not touch the eye)
Repeat with the upper eyelid, rolling your finger downward in a rolling motion.
Lid Scrubs
Purpose: Remove the lid crusting/debris to decrease the amount of bacteria and dead skin cells exposed to the ocular surface. Helps maintain clean lids/lashes.
Instructions
Mix warm water and a small amount of non irritating (baby) shampoo
Using a clean cloth, rub the solution back and forth across the eyelashes and the edge of the closed eyelid, being careful not to get it in the eye
Then with another clean cloth, start at the base of the lashes and wipe outward, trying to remove the lid crusting away from the eyes. Can also use a cue tip, especially for the lower eyelashes
Rinse with clear water
Repeat with the other eye.
Alternatively, purchase lid scrubs at the store (no prescription required). Start at the base of the lashes / eyelid and cleanse the upper and lower lids. To save on eyelid scrubs, try cutting them in half.
Eye Drops
Talk to your eye doctor about which eye drops are most appropriate for your child.
Artificial tears
Refresh, Systane, Blink, and TheraTears (use of up to 4 times per day); come in small bottles
Non-Preserved Refresh, Systane, Blink drops (come in single use vials, can use as many times per day but throw away after 24 hours)
Allergy eye drops (only 1 required)
Olopatadine 0.2% or 0.7% (extra strength): 1 drop in each eye once a day
Lastacaft 0.025%: 1 drop in each eye once a day
Ketotifen 0.025%: 1 drop in each eye eye twice a day (also known as Zaditor, Alaway, Claritin)
Stay away from drops that contain the ingredient: tetrahydrozoline or naphazoline (such as in Visine or Clear Eyes). These drops constrict the blood vessels on the ocular surface (which is how they decrease redness) however, people can become dependent on these drops and get redness when they stop taking the drops. Additionally, these ingredients do not help with treating the underlying cause of the inflammation and mask the symptoms.
Antibiotics and steroid drops or ointments (prescription only). Antibiotic drops or ointment along with steroid drops can be useful in calming down any eye inflammation. This may be indicated if there is significant inflammation affecting the cornea of the eyes due to the risk of corneal scarring and infection. However, we want to avoid staying on the steroid for too long since they are associated with bad side effects with prolonged use. Your eye doctor will discuss with you whether this treatment is suitable and provide you with more specific instructions regarding this treatment.
Optional Treatment- Omega 3 fatty acids
Omega 3 fatty acids can also be incorporated into the diet. This may be through food (fish and other seafood, nuts, flaxseed oil, etc). They are also readily available in supplements (including gummies). However, the scientific evidence of their benefit in blepharitis treatment is still debated so this treatment is optional.
Remember
Unfortunately, due to the chronic nature of BKC, you should expect to maintain a consistent lid hygiene treatment for a couple of years (children may outgrow this condition in late teens/early twenties)
Make sure to call your eye doctor’s office and/or schedule an appointment as soon as possible if your child’s condition worsens (they experience pain, light sensitivity, redness, a decrease in vision, etc) as these could be signs of an inflammatory episode where more aggressive treatment is warranted
Follow up with your eye doctor on at least a yearly basis